Practice Essentials
Lupus nephritis is clinically evident in 50-60% of patients with systemic lupus erythematosus (SLE), and it is histologically evident in most SLE patients, even those without clinical manifestations of kidney disease. (See the image below.) Evaluating kidney function in SLE patients is important because early detection and treatment of kidney involvement can significantly improve renal outcome.
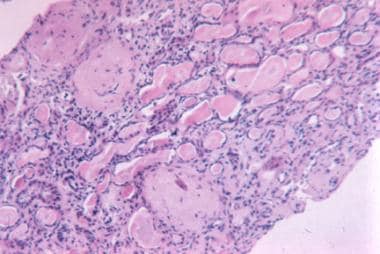 Advanced sclerosis lupus nephritis. International Society of Nephrology/Renal Pathology Society 2003 class VI (×100, hematoxylin-eosin).
Advanced sclerosis lupus nephritis. International Society of Nephrology/Renal Pathology Society 2003 class VI (×100, hematoxylin-eosin).
Signs and symptoms
Patients with lupus nephritis may report other symptoms of active SLE (eg, fatigue, fever, rash, arthritis, serositis, or central nervous system [CNS] disease); these are more common with focal (proliferative) and diffuse (proliferative) lupus nephritis.
Asymptomatic lupus nephritis
-
During regular follow-up, laboratory abnormalities suggesting active lupus nephritis include hematuria or proteinuria; this is more typical of mesangial or membranous lupus nephritis.
Active nephritis
Nephritic symptoms related to hypertension and poor kidney function (typical of diffuse lupus nephritis):
-
Peripheral edema
-
Headache and dizziness
-
Nausea and vomiting
Nephrotic symptoms related to proteinuria (ypical of membranous lupus nephritis):
-
Peripheral or periorbital edema
-
Coagulopathy
Physical findings
-
Focal and diffuse lupus nephritis – Generalized active SLE with the presence of a rash, oral or nasal ulcers, synovitis, or serositis; signs of active nephritis
-
Active lupus nephritis – Hypertension; peripheral edema; and, occasionally, cardiac decompensation
-
Membranous lupus nephritis – Peripheral edema, ascites, and pleural and pericardial effusions without hypertension
See Presentation for more detail.
Diagnosis
Laboratory tests to evaluate kidney function in SLE patients include the following:
-
Blood urea nitrogen (BUN) testing
-
Serum creatinine assessment
-
Urinalysis (to check for protein, red blood cells [RBCs], and cellular casts)
-
Spot urine test for creatinine and protein concentration
-
24-hour urine test for creatinine clearance and protein excretion
Laboratory tests for SLE disease activity include the following:
-
Antibodies to double-stranded DNA (dsDNA)
-
Complement (C3, C4, and CH50)
-
Erythrocyte sedimentation rate (ESR)
-
C-reactive protein (CRP)
Kidney biopsy should be considered in any patient with SLE who has clinical or laboratory evidence of active nephritis, especially upon the first episode of nephritis.
Lupus nephritis is staged according to the classification revised by the International Society of Nephrology (ISN) and the Renal Pathology Society (RPS) in 2003, as follows:
-
Class I – Minimal mesangial lupus nephritis
-
Class II – Mesangial proliferative lupus nephritis
-
Class III – Focal lupus nephritis (active and chronic; proliferative and sclerosing)
-
Class IV – Diffuse lupus nephritis (active and chronic; proliferative and sclerosing; segmental and global)
-
Class V – Membranous lupus nephritis
-
Class VI – Advanced sclerosis lupus nephritis
See Workup for more detail.
Management
The principal goal of therapy in lupus nephritis is to normalize kidney function or, at least, to prevent the progressive loss of kidney function. Therapy differs, depending on the pathologic lesion.
Key points of American College of Rheumatology guidelines for managing lupus nephritis are as follows:
-
Patients with clinical evidence of active, previously untreated lupus nephritis should have a kidney biopsy to classify the disease according to ISN/RPS criteria
-
All patients with lupus nephritis should receive background therapy with hydroxychloroquine, unless contraindicated
-
Glucocorticoids plus either cyclophosphamide intravenously or mycophenolate mofetil orally should be administered to patients with class III/IV disease; patients with class I/II nephritis do not require immunosuppressive therapy
-
Angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers should be administered if proteinuria reaches or exceeds 0.5 g/day
-
Blood pressure should be maintained at or below 130/80 mm Hg
Patients with class V lupus nephritis are generally treated with prednisone for 1-3 months, followed by tapering for 1-2 years if a response occurs. If no response occurs, the drug is discontinued. Immunosuppressive drugs are generally not used unless kidney function worsens or a proliferative component is present on kidney biopsy samples.
Newer therapies for lupus nephritis include the following:
-
The oral calcineurin inhibitor voclosporin, which is approved for use in conjunction with immunosuppressive treatment
-
Belimumab, an anti–B-lymphocyte stimulator [BLyS] monoclonal antibody, which is approved for treatment of adults with active lupus nephritis who are receiving standard therapy
Investigational therapies for lupus nephritis and SLE include the following:
-
Rituximab
-
Other anti-CD20 monoclonal antibodies (eg, ocrelizumab, ofatumumab, epratuzumab, and TRU-015)
-
Atacicept
-
Abetimus
-
Anticytokine therapies (eg, monoclonal antibodies directed against interferon alfa, interleukin [IL]-1, IL-6, IL-10, and tumor necrosis factor alpha [TNF-α])
Patients with end-stage renal disease require dialysis and are good candidates for kidney transplantation. Hemodialysis is preferred to peritoneal dialysis.
See Treatment and Medication for more detail.
For patient education information, see Lupus Nephritis.
Pathophysiology
Autoimmunity plays a major role in the pathogenesis of lupus nephritis. The immunologic mechanisms include production of autoantibodies directed against nuclear elements. Characteristics of the nephritogenic autoantibodies associated with lupus nephritis are as follows [1] :
-
Antigen specificity directed against nucleosome or double-stranded DNA (dsDNA) - Some anti-dsDNA antibodies cross-react with the glomerular basement membrane
-
Higher-affinity autoantibodies may form intravascular immune complexes, which are deposited in glomeruli
-
Cationic autoantibodies have a higher affinity for the anionic glomerular basement membrane
-
Autoantibodies of certain isotypes (immunoglobulin [Ig] G1 and IgG3) readily activate complement
These autoantibodies form pathogenic immune complexes intravascularly, which are deposited in glomeruli. Alternatively, autoantibodies may bind to antigens already located in the glomerular basement membrane, forming immune complexes in situ. Immune complexes promote an inflammatory response by activating complement and attracting inflammatory cells, including lymphocytes, macrophages, and neutrophils. [2, 3]
The histologic type of lupus nephritis that develops depends on numerous factors, including the antigen specificity and other properties of the autoantibodies and the type of inflammatory response that is determined by other host factors. In more severe forms of lupus nephritis, proliferation of endothelial, mesangial, and epithelial cells and the production of matrix proteins lead to fibrosis. [4]
Glomerular thrombosis is another mechanism that may play a role in pathogenesis of lupus nephritis, mainly in patients with antiphospholipid antibody syndrome, and is believed to be the result of antibodies directed against negatively charged phospholipid-protein complexes. [2]
Specific strains of a gut commensal may contribute to the immune pathogenesis of lupus nephritis. Azzouz and colleagues analyzed blood and fecal samples from 61 women with SLE and 17 healthy women. On rRNA amplification analysis, patients with SLE displayed a fivefold higher number of Gram-positive fecal bacteria, specifically Ruminococcus gnavus (RG). When the researchers stratified patients with SLE according to organ involvement, those with a history of kidney disease demonstrated an abundance of RG-specific amplicon sequence variant compared with those who had no renal impairment. [5]
Etiology
Genetic factors
As with many autoimmune disorders, evidence suggests that genetic predisposition plays an important role in the development of both SLE and lupus nephritis. Multiple genes, many of which are not yet identified, mediate this genetic predisposition (see Table 1 below). [6, 7, 8, 9, 4, 10]
Table 1. Genes Associated With Systemic Lupus Erythematosus (Open Table in a new window)
Gene Locus |
Gene Name |
Gene Product |
1p13.2 |
PTPN22 |
Lymphoid-specific protein tyrosine phosphatase |
1q21-q23 |
CRP |
CRP |
1q23 |
FCGR2A, FCGR2B |
FcγRIIA (R131), FcγRIIB |
1q23 |
FCGR3A, FCGR3B |
FcγRIIIA (V176), FcγRIIIB |
1q31-q32 |
IL10 |
IL-10 |
1q36.12 |
C1QB |
C1q deficiency |
2q32.2-q32.3 |
STAT4 |
Signal transducer and activator of transcription 4 |
2q33 |
CTLA4 |
Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) |
6p21.3 |
HLA-DRB1 |
HLA-DRB1: DR2/*1501, DR3/*0301C1q deficiency |
6p21.3 |
C2, C4A, C4B |
C2, C4 deficiencies |
6p21.3 |
TNF |
TNF-a (promoter, -308) |
10q11.2-q21 |
MBL2 |
Mannose-binding lectin |
CRP = C-reactive protein; HLA = human leukocyte antigen; IL = interleukin; TNF = tumor necrosis factor. |
||
SLE is more common in first-degree relatives of patients with SLE (familial prevalence, 10-12%). Concordance rates are higher in monozygotic twins (24-58%) than in dizygotic twins (2-5%), supporting an important role for genetics in the development of SLE. However, the concordance rate in monozygotic twins is not 100%, suggesting that environmental factors trigger development of clinical disease.
Human leukocyte antigen (HLA) class II genes include the following:
-
HLA-DR2 and HLA-DR3 are associated with SLE
-
HLA-DR4 is associated with a lower prevalence of SLE and appears to be protective
Complement genes include the following:
-
C1Q, C1R, and C1S deficiencies are associated with SLE, lupus nephritis, and production of anti-dsDNA
-
C2 and C4 deficiencies are associated with SLE or lupus-like syndrome
-
C4A and C4B (possibly) gene deletions are associated with SLE
FcγR genes include the following:
-
These mediate the binding of IgG and IgG-containing immune complexes to cells such as macrophages and other mononuclear phagocytes
-
FcγRIIa binds to IgG2 and is encoded by 2 codominant alleles, H131 (or high affinity) and R131 (or low affinity); the low-affinity phenotype (homozygous for R131 allele; 131R/R) is associated with lupus nephritis in African Americans
-
FcγRIIIa binds to IgG1 and is encoded by 2 codominant alleles, V158 (or high affinity) and F158 (or low affinity); the low-affinity phenotype (homozygous for F158 allele; 158F/F) is associated with SLE
Other relevant genes include the following:
-
Cytokine genes - Certain polymorphisms of the IL10 gene (high producers) and possibly the IL1RN and TNFA genes (low producers) are associated with SLE
-
Mannose-binding lectin genes - These gene polymorphisms are associated with an increased risk of SLE
-
Apoptosis genes - Defects of several apoptosis genes are associated with lupuslike syndromes in mice and, rarely, SLE in humans, including CD95 (Fas) and CD178 (FasL)
Immunologic factors
The initial autoantibody response appears to be directed against the nucleosome, which arises from apoptotic cells. [4, 11, 12]
Patients with SLE have poor clearance mechanisms for cellular debris. Nuclear debris from apoptotic cells induces plasmacytoid dendritic cells to produce interferon-α, which is a potent inducer of the immune system and autoimmunity. [13, 14, 15]
Autoreactive B lymphocytes, which are normally inactive, become active in SLE because of a malfunction of normal homeostatic mechanisms, resulting in escape from tolerance. This leads to the production of autoantibodies. Other autoantibodies, including anti-dsDNA antibodies, develop through a process of epitope spreading. These autoantibodies develop over time, in an orderly fashion, months to years before the onset of clinical SLE. [16]
Epidemiology
Frequency
In a multi-ethnic international cohort of patients enrolled within 15 months (mean, 6 months) after SLE diagnosis and assessed annually, lupus nephritis occurred in 700 of 1827 patients (38.3%). Lupus nephritis was frequently the initial presentation of SLE; it was identified at enrollment in 80.9% of cases. Patients with nephritis were younger, more frequently men and of African, Asian, and Hispanic race/ethnicity. [17]
In a study of a large Spanish registry, lupus nephritis was histologically confirmed in 1092 of 3575 patients with SLE (30.5%). The mean age at lupus nephritis diagnosis was 28.4 years. The risk for lupus nephritis development was significantly higher in men, in younger individuals, and in Hispanics. Patients receiving antimalarials had a significantly lower risk of developing lupus nephritis. [18]
Age-related demographics
Most patients with SLE develop lupus nephritis early in their disease course. SLE is more common among women in the third decade of life, and lupus nephritis typically occurs in patients aged 20-40 years. [19] Children with SLE are at a higher risk of renal disease than adults and tend to sustain more disease damage secondary to more aggressive disease and treatment-associated toxicity. [20, 21, 22]
Sex-related demographics
Because the overall prevalence of SLE is higher in females (ie, female-to-male ratio of 9:1), lupus nephritis is also more common in females; however, clinical renal disease has a worse prognosis and is more common in males with SLE. [19]
Race-related demographics
SLE is more common in African Americans and Asians than in white people, with the highest prevalence in Caribbean people. The prevalence of lupus nephritis is much higher in Asians than in Whites with SLE, but the 10-year renal outcome and renal survival rate appear to be better in Asians. [23] Particularly severe lupus nephritis may be more common in African Americans and Asians than in other ethnic groups. [19]
Prognosis
Over the past 4 decades, changes in the treatment of lupus nephritis and general medical care have greatly improved both renal involvement and overall survival. During the 1950s, the 5-year survival rate among patients with lupus nephritis was close to 0%. The subsequent addition of immunosuppressive agents such as intravenous (IV) pulse cyclophosphamide has led to documented 5- and 10-year survival rates as high as 85% and 73%, respectively. [24]
Mortality in patients with end-stage renal disease due to lupus nephritis has declined significantly in recent decades. The mortality rate per 100 patient-years declined from 11.1 in 1995-1999 to 6.7 in 2010-2014. Deaths due to cardiovascular disease declined by 44% and deaths due to infection declined 63%. [25]
Morbidity associated with lupus nephritis is related to the renal disease itself, as well as to treatment-related complications and comorbidities, including cardiovascular disease and thrombotic events. Progressive renal failure leads to anemia, uremia, and electrolyte and acid-based abnormalities. Hypertension may lead to an increased risk of coronary artery disease and cerebrovascular accident.
Nephrotic syndrome may lead to edema, ascites, and hyperlipidemia, adding to the risk of coronary artery disease and the potential for thrombosis. The findings from one study indicate that patients with lupus nephritis, particularly early-onset lupus nephritis, are at increased risk for morbidity from ischemic heart disease. [26]
In a study of 56 children (< 18 years) with either global or segmental diffuse proliferative lupus nephritis, long-term renal outcomes were similar. Most patients reached adulthood but sustained significant renal damage. Complete remission rates were 50% and 60% in the global and segmental groups, respectively. Renal survival rates, defined as an estimated glomerular filtration rate of ≥60 mL/min/1.73 m2, were 93%, 78%, and 64 % at 1, 5, and 10 years, respectively, and corresponding patient survival rates were 98%, 96%, and 91%, respectively, with similar rates in the global and segmental groups. [27]
Therapy with corticosteroids, cyclophosphamide, and other immunosuppressive agents increases the risk of infection. Long-term corticosteroid therapy may lead to osteoporosis, avascular necrosis, diabetes mellitus, and hypertension, among other complications. Cyclophosphamide therapy may cause cytopenias, hemorrhagic cystitis, infertility, and an increased risk of malignancy.
Biomarkers of renal outcome in lupus nephritis include proteinuria and serum albumin. Studies have shown that a proteinuria cut-off of less than 0.7 or 0.8 g/day at 12 months predicts good long-term renal outcome. Domingues et al reported that serum albumin > 3.7 g/dL at 12 months predicts favorable renal outcome at 48 months. [28]
-
Mesangial proliferative lupus nephritis with moderate mesangial hypercellularity. International Society of Nephrology/Renal Pathology Society 2003 class II (×200, hematoxylin-eosin).
-
Focal lupus nephritis. International Society of Nephrology/Renal Pathology Society 2003 class III (×100, hematoxylin-eosin).
-
Focal lupus nephritis. International Society of Nephrology/Renal Pathology Society 2003 class III (×200, immunofluorescence).
-
Diffuse lupus nephritis with hypertensive vascular changes. International Society of Nephrology/Renal Pathology Society 2003 class IV (×200, hematoxylin-eosin).
-
Diffuse lupus nephritis with early crescent formation. International Society of Nephrology/Renal Pathology Society 2003 class IV (×200, hematoxylin-eosin).
-
Diffuse lupus nephritis with extensive crescent formation (rapidly progressive glomerulonephritis). International Society of Nephrology/Renal Pathology Society 2003 class IV (×200, hematoxylin-eosin).
-
Membranous lupus nephritis. International Society of Nephrology/Renal Pathology Society 2003 class V (×200, hematoxylin-eosin).
-
Membranous lupus nephritis showing thickened glomerular basement membrane. International Society of Nephrology/Renal Pathology Society 2003 class V (×200, silver stain).
-
Advanced sclerosis lupus nephritis. International Society of Nephrology/Renal Pathology Society 2003 class VI (×100, hematoxylin-eosin).







