Practice Essentials
Sialadenitis of the submandibular gland is a relatively commonly encountered yet infrequently discussed topic. Causes range from simple infection to autoimmune etiologies. Although not as frequent as sialadenitis of the parotid gland, it represents an important area of clinical relevance to the otolaryngologist and other specialists. The following discusses the basic science of the submandibular gland, as well as the more common causes of sialadenitis and sialadenosis of the submandibular gland. [1]
Anatomy
The submandibular gland, along with the parotid and sublingual glands, comprise the major salivary glands. The minor salivary glands are scattered along the upper aerodigestive tract, including the lips, mucosa of the oral cavity, pharynx, and hard palate.
The submandibular gland is the second largest (approximate weight, 10 g) of the major salivary glands (the parotid gland is the largest). Anatomically, it is situated in the submandibular triangle of the neck.
The gland itself can be arbitrarily divided into superficial and deep lobes based on its relationship to the mylohyoid muscle, the former lying superficial to the muscle, and the latter wrapping around the posterior aspect of the muscle. The gland itself lies on the hyoglossus muscle, superficial to both the hypoglossal and the lingual nerves, the latter supplying parasympathetic innervation by way of the chorda tympani nerve (from cranial nerve VII) and the submandibular ganglion. The duct of the submandibular gland, also known as the Wharton duct, exits the gland from the deep lobe, passing through the floor of the mouth, and opening in close proximity to the lingual frenulum. See the image below.
Diagnosis and management of submandibular sialadenitis/sialadenosis
In evaluating the patient with sialadenitis, steps should be taken in the following order: history, physical examination, culture, laboratory investigation, radiography, and if indicated, fine-needle aspiration biopsy (see History and Physical).
Management of submandibular sialadenitis and sialadenosis involves a wide range of approaches, from conservative medical management to more aggressive surgical intervention.
One management scheme is as follows:
-
Acute sialadenitis - Medical management (hydration, antibiotics [oral versus parenteral], warm compresses and massage, sialogogues); [2] surgical management (consideration of incision and drainage versus excision of the gland in cases refractory to antibiotics, incision and drainage with abscess formation, gland excision in cases of recurrent acute sialadenitis)
-
Salivary calculi - Medical management (hydration, compression and massage, antibiotics for the infected gland); surgical management (duct cannulation with stone removal, gland excision in recurrent case)
-
Sjögren disease - Medical management (hydration, dental hygiene, rheumatology and dental referral); surgical management (gland excision not usually needed unless recurrent acute sialadenitis)
-
Sialadenosis - medical management (treatment of underlying cause); surgical management (not indicated)
Pathophysiology
The salivary glands serve numerous functions, including lubrication; enzymatic degradation of food substances; production of hormones, antibodies, and other blood group–reactive substances; mediation of taste; and antimicrobial protection. The regulation of salivary flow is primarily through the autonomic system and, most importantly, the parasympathetic division. In the case of the submandibular gland, this is mediated through the submandibular ganglion. Presynaptic fibers are derived from the superior salivatory nucleus and carried by the chorda tympani nerve, which joins the lingual nerve traveling towards the ganglion. Postsynaptic fibers extend from the ganglion to the gland itself.
Saliva is produced in the glandular subunit. The fluid component of the saliva is derived from the perfusing blood vessels in proximity to the gland, while the macromolecular composition is derived from secretory granules within the acinar cells. The saliva is produced in the acinus. Myoepithelial cells, containing contractile elements, are located along the periphery of the acinus. Upon contraction of these myoepithelial cells, the saliva is secreted into the ductal system.
The exact mechanism of salivary secretion is not completely understood but is believed to be under the influence of a cyclic AMP (adenosine 3,'5'-cyclic monophosphate) and a calcium-activated phosphorylation mechanism. The salivary secretions are then modified by a variety of cell types along a series of ducts, including the striated, intercalated, and excretory ducts, before finally being excreted through the Wharton duct into the oral cavity.
The concentration of mucus is higher in the submandibular gland, accounting for the viscous nature of its secretions relative to the other salivary glands. This increased viscosity, and subsequent relatively slower flow, contributes to the propensity for salivary gland calculi and stasis in certain disease states.
Epidemiology
Frequency
United States
The exact frequency of submandibular sialadenitis is unclear. The incidence of acute suppurative parotitis has been reported at 0.01-0.02% of all hospital admissions. The submandibular gland is suggested to account for approximately 10% of all cases of sialadenitis of the major salivary glands. Extrapolation would suggest an incidence of 0.001-0.002%, but this is unconfirmed.
Race
No race predilection per se exists.
Sex
No sex predilection per se exists.
Age
Although no obvious age predilection exists, per se, sialadenitis as a whole tends to occur in the older, debilitated, or dehydrated patient. [3]
-
Submandibular calculus.
-
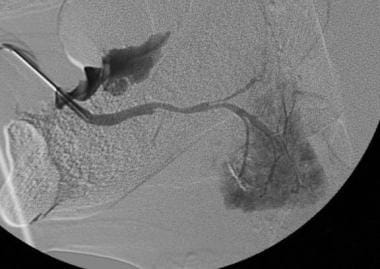
Sialogram with stenosis secondary to chronic sialadenosis.
-
Submandibular abscess and associated Ludwig angina.
-
Submandibular neoplasm.