Practice Essentials
Diaper rash, or diaper dermatitis, is a general term describing any of a number of inflammatory skin conditions that can occur in the diaper area. [1] (See the image below.) These disorders can be conceptually divided into 3 categories:
-
Rashes that are directly or indirectly caused by the wearing of diapers: This category includes dermatoses, such as irritant contact dermatitis, miliaria, intertrigo, candidal diaper dermatitis, and granuloma gluteale infantum.
-
Rashes that appear elsewhere but can be exaggerated in the groin area due to the irritating effects of wearing a diaper: This category includes atopic dermatitis, seborrheic dermatitis, and psoriasis.
-
Rashes that appear in the diaper area irrespective of diaper use: This category includes rashes associated with bullous impetigo; Langerhans cell histiocytosis (Letterer-Siwe disease, a rare and potentially fatal disorder of the reticuloendothelial system); acrodermatitis enteropathica (zinc deficiency); congenital syphilis; scabies; and HIV.
Allergic contact dermatitis is exceedingly rare in the infant and is not discussed here. The focus of this article is on the pathophysiology, diagnosis, and treatment of the rashes in the first category. By definition, these are truly diaper rashes because they present as a rash in the diaper area and can be cured by a change in diapering practices. The dermatoses within the other 2 categories do not typically appear as a diaper rash alone, and they do not necessarily respond to diapering modifications. These more generalized diseases are mentioned in terms of helping the emergency physician make the correct diagnosis. However, details about their etiology and management are beyond the scope of this article.
Pathophysiology
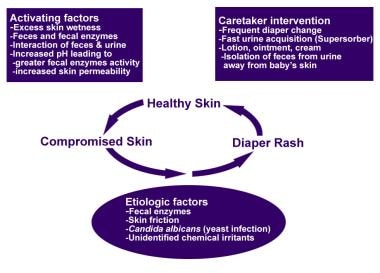
The precise etiology of most diaper rashes is not clearly defined. They likely result from a combination of factors that includes wetness, friction, urine and feces, and the presence of microorganisms. Anatomically, this skin region features numerous folds and creases, which present a problem with regard to both efficient cleansing and control of the microenvironment.
The main irritants in this situation are fecal proteases and lipases, whose activity is increased greatly by elevated pH. An acidic skin surface is also essential for the maintenance of the normal microflora, which provides innate antimicrobial protection against invasion by pathogenic bacteria and yeasts. Fecal lipase and protease activity is also greatly increased by acceleration of gastrointestinal transit; this is the reason for the high incidence of irritant diaper dermatitis observed in babies who have had diarrhea in the previous 48 hours.
The wearing of diapers causes a significant increase in skin wetness and pH. Prolonged wetness leads to maceration (softening) of the stratum corneum, the outer, protective layer of the skin, which is associated with extensive disruption of intercellular lipid lamellae. A series of diaper studies conducted mainly in the late 1980s found a significant decrease in skin hydration following the introduction of diapers with a superabsorbent core. [2] Recent studies confirm that this trend is ongoing. [3, 4, 5] Weakening of its physical integrity makes the stratum corneum more susceptible to damage by (1) friction from the surface of the diaper and (2) local irritants.
The cycle of diaper rash is shown in the illustration below.
At full term, the skin of infants is an effective barrier to disease and is equal to adult skin with regard to permeability. Some studies reported infant's transepidermal water loss to be lower than that of adult skin. However, dampness, lack of air exposure, acidic or irritant exposures, and increases in skin friction begin to break down the skin barrier.
The normal pH of the skin is between 4.5 and 5.5. When urea from the urine and stool mix, urease breaks down the urine, decreasing the hydrogen ion concentration (increasing pH). Elevated pH levels increase the hydration of the skin and make the skin more permeable.
Previously, ammonia was believed to be the primary cause of diaper dermatitis. Recent studies have disproved this, showing that when ammonia or urine is placed on the skin for 24-48 hours, no apparent skin damage occurs.
A series of studies has shown that the pH of cleansing products can change the microbiological spectrum of the skin. [6, 7] High soap pH values encourage propionibacterial growth on skin, whereas syndets (ie, synthetic detergents) with a pH of 5.5 did not cause changes in the microflora. A study looked to explain the relationship between skin barrier function in 4-day-old infants and the occurrence of diaper dermatitis during the first month of life. The study concluded that early neonatal skin pH may predict the risk of diaper dermatitis during the first month of life. These results may be useful in devising strategies to prevent diaper dermatitis. [8]
Miliaria
Obstruction of eccrine sweat glands when the stratum corneum becomes excessively hydrated and edematous is believed to cause miliaria.
Intertrigo
Intertrigo occurs when wet skin, which is more fragile and has a higher coefficient of friction, becomes damaged from maceration and chafing.
Contact dermatitis
Irritant contact dermatitis is most likely made up of some combination of intertrigo and miliaria. In addition, it has been shown to result from the irritating effects of mixing urine with feces. Urine in the presence of fecal urease becomes more alkaline due to the production of ammonia. This alkaline urine causes activation of fecal lipases, ureases, and proteases. These, in turn, irritate the skin directly and increase its permeability to other low molecular weight irritants.
Candidal diaper dermatitis
Once the skin is compromised, secondary infection by Candida albicans is common. Between 40% and 75% of diaper rashes that last for more than 3 days are colonized with C albicans. Candida has a fecal origin and is not an organism normally found on perineal skin. Amoxicillin was found to increase the colonization by Candida and worsens the diaper dermatitis.
A study by Ersoy-Evans et al of 63 infants with diaper rash found that those with Candida infection (77.4% of the patients) had a significantly greater median number of previous diaper rash episodes than did those with noncandidal diaper rash. [9]
Bacterial diaper dermatitis
Bacteria may play a role in diaper dermatitis through reduction of fecal pH and the resultant activation of enzymes. Additionally, fecal microorganisms probably contribute to secondary infections when they occur. This is particularly evident with bullous impetigo in the diaper area, which causes bullae that are flaccid but sometimes tense due to Staphylococcus aureus infection, or a cellulitis due to cutaneous streptococci, or even a folliculitis due to S aureus infection.
Polymicrobial growth is documented in at least half of diaper rash cultures. Staphylococcus species are the most commonly grown organisms, followed by Streptococcus species and organisms from the family Enterobacteriaceae. Nearly 50% of isolates also contain anaerobes.
Granuloma gluteale infantum
Granuloma gluteale infantum is a rare disorder. [10] It is not very well understood, but it probably represents an unusual inflammatory response to long-standing irritation, candidiasis, or fluorinated corticosteroids.
Etiology
A precise etiology of common diaper rashes has not been determined. Rashes have been associated with the following:
-
Infrequent diaper changes
-
Improper cleansing and drying of the diaper area
-
Failure to apply topical preparations to protect the skin
-
Diarrhea
Candida is a common cause of secondary infection. Other possible sources of secondary infection include species of Staphylococcus, Streptococcus, and enteric anaerobes (Bacteroides and Peptostreptococcus species).
The aforementioned study by Ersoy-Evans et al, of 63 infants with diaper rash, found significantly fewer previous instances of the condition in breastfed babies. [9]
Epidemiology
United States statistics
Diaper rash is the most common dermatitis found in infancy. Prevalence has been variably reported from 4-35% in the first 2 years of life. Incidence triples in babies with diarrhea. It is not unusual for every child to have at least 1 episode of diaper rash by the time he or she is toilet-trained. [11]
Because fewer than 10% of all diaper rashes are reported by the family, the actual incidence of this condition is likely underestimated if office visits are used as the screening site.
The incidence is lower among breastfed infants [12] —perhaps due to the less acidic nature of their urine and stool.
Babies wearing superabsorbent disposable diapers with a central gelling material have fewer episodes of diaper dermatitis compared with their counterparts wearing cloth diapers. However, keep in mind, that superabsorbent diapers contain dyes that were suspected to cause allergic contact dermatitis (ACD). One study reviewed the effect on the skin of dye-free diapers as compared with dye-containing diapers. [13] A patch testing result with dye similar to that in diapers was positive in 2 out of 4 patients. This study also reported improvement with dye-free diapers for all of the patients. This would support the hypotheses that these children had allergic contact dermatitis attributable to the various dyes in the diapers. The patterns of eruption and the responses to dye-free diapers support a diagnosis of allergic contact dermatitis. Colors are added to diapers primarily for aesthetic purposes or absorbency potential.
International statistics
Few investigations have been reported regarding prevalence outside of the United States. However, one study performed in Italy showed a prevalence of 15.2%, and a peak incidence of 19.4% in those aged 3-6 months. [14]
One large British study reported diaper dermatitis in 25% of children aged 1 month.
A Nigerian study conducted in 1995-1996 identified diaper dermatitis in 7% of children.
A study in Kuwait noted that diaper dermatitis occurs in 4% of pediatric dermatology cases.
These studies do not distinguish between common or generic diaper dermatitis and secondary diaper dermatitis.
Race-, sex-, and age-related demographics
Atopic dermatitis and related diaper dermatitis are more common among African American patients.
No sexual predilection exists.
Diaper rashes can start in the neonatal period as soon as the child begins to wear diapers. The incidence peaks in those aged 7-12 months, then decreases with age. Diaper rash stops being a problem once the child is toilet trained, usually around age 2 years.
Prognosis
Most cases completely resolve after a concerted effort by the parents toward diaper hygiene. The time to resolution is typically a few days for uncomplicated irritant dermatitis, intertrigo, and miliaria.
Candidal infections last a few weeks after treatment is begun. A study by Adalat et al showed that oral thrush was present in 5% of children and had a strongly significant association with a current episode of diaper dermatitis. [15]
At least one half of the cases of atopic dermatitis resolve by the third year of life. Granuloma gluteale infantum tends to resolve spontaneously over the course of a few months. Langerhans cell histiocytosis is usually a fatal disease.
Morbidity/mortality
This disease is not usually life threatening; however, it may cause significant distress for parents. Morbidity for the child mostly is in the form of pain and itching in the affected areas. In one report, diaper rash accounted for nearly 20% of pediatric office visits.
Complications
Because of maceration and abrasion of the skin under the diaper, skin ulceration and secondary infection by C albicans or bacteria are common. Prevalence of a secondary bacterial infection is uncertain, but it is frequent. Multiple organisms, both aerobic and anaerobic, contribute to the development of this condition.
Psoriasis id reaction refers to a psoriaticlike eruption of papules and plaques after the initiation of treatment to a candidal infection. The following are common characteristics:
-
Involves the torso and the upper body and usually spares the extremities
-
Occurs days after antifungal therapy is started
-
Is poorly understood but can be treated with low or intermediate potency steroids
Jacquet dermatitis is a complicated form of the irritant chafing type of diaper rash. The following are typical features:
-
It involves the development of erosive ulcerations with elevated margins.
-
Some nodular patterns also are described in severe chronic irritant dermatitis.
-
Cases remain surprisingly asymptomatic and usually are not secondarily infected.
Psoriasiform napkin dermatitis refers to a clinical presentation that combines features of seborrheic and candidal diaper rashes. Secondary bacterial and yeast infections can occur.
Patient Education
The parents of the patient should be educated about proper diaper hygiene and the need for frequent diaper changes to prevent future episodes.
Parents should be taught how to recognize changes in the rash indicative of a secondary infection and should be advised to seek medical attention in such instances.
For patient education resources, see the Children's Health Center, as well as Diaper Rash, Skin Rashes in Children, and Yeast Infection Diaper Rash.
-
Diaper rash.
-
Diaper rash.
-
Diaper rash.
-
Diaper rash pathophysiology scheme.