Background
Cluster headache (CH), also known as histamine headache, is a primary neurovascular headache disorder, the pathophysiology and etiology of which are not well understood. [1] As the name suggests, CH involves a grouping of headaches, usually over a period of several weeks. According to the diagnostic criteria developed by the International Headache Society (IHS), CH has the following characteristics: [2, 3]
-
The patient experiences attacks of severe or very severe, strictly unilateral pain (orbital, supraorbital, or temporal pain) that last 15-180 minutes and occur from once every other day to 8 times a day
-
The attacks are associated with 1 or more of the following (all ipsilateral): conjunctival injection, lacrimation, nasal congestion, rhinorrhea, forehead and facial sweating, miosis, ptosis, or eyelid edema
CH may be usefully classified into 2 main forms as follows:
-
Episodic CH, in which at least 2 cluster phases lasting 7 days to 1 year are separated by pain-free periods lasting at least 3 months
-
Chronic CH, in which the clusters occur for one year or longer without remission, or with remissions lasting less than 3 months
Pathophysiology
The underlying pathophysiology of cluster headache (CH) is incompletely understood. [4, 5] The periodicity of the attacks suggests the involvement of a biologic clock within the hypothalamus (which controls circadian rhythms), with central disinhibition of the nociceptive and autonomic pathways—specifically, the trigeminal nociceptive pathways. Positron emission tomography (PET) and voxel-based morphometry have identified the posterior hypothalamic gray matter as the key area for the basic defect in CH. [1] See the images below.
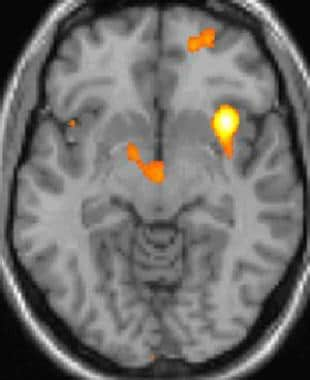 Cluster headache: Functional imaging shows activation of specific brain areas during pain. Courtesy of Wikipedia Commons.
Cluster headache: Functional imaging shows activation of specific brain areas during pain. Courtesy of Wikipedia Commons.
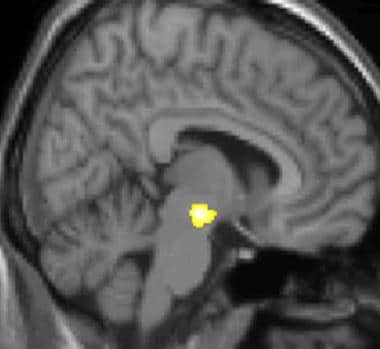 Cluster headache (CH): Voxel-based morphometry (VBM) structural imaging shows specific brain area of CH patients' (hypothalamus) being different to non-CH patients' brains. Courtesy of Wikipedia Commons.
Cluster headache (CH): Voxel-based morphometry (VBM) structural imaging shows specific brain area of CH patients' (hypothalamus) being different to non-CH patients' brains. Courtesy of Wikipedia Commons.
Altered habituation patterns and changes have been observed within the trigeminal-facial neuronal circuitry secondary to central sensitization, in addition to dysfunction of the serotonergic raphe nuclei-hypothalamic pathways (though the latter is not as striking as in migraine). Functional hypothalamic dysfunction has been confirmed by abnormal metabolism based on the N-acetylaspartate neuronal marker in magnetic resonance spectroscopy. [6]
Substance P neurons carry sensory and motor impulses in the maxillary and ophthalmic divisions of the trigeminal nerve. These connect with the sphenopalatine ganglion and interior carotid perivascular sympathetic plexus. Somatostatin inhibits substance P and reduces the duration and intensity of CH.
Vascular dilatation may play a role in the pathogenesis of CH, but blood flow studies are inconsistent. Extracranial blood flow (hyperthermia and increased temporal artery blood flow) increases, but only after the onset of pain. Vascular change is considered secondary to primary neuronal discharge.
Although the evidence supporting a causative role for histamine is inconsistent, cluster headaches may be precipitated with small amounts of histamine. Antihistamines do not abort cluster headaches. Increased numbers of mast cells have been found in the skin of painful areas of some patients, but this finding is inconsistent.
Etiology
The exact cause of cluster headache (CH) is unknown. The disorder is sporadic, though rare cases of an autosomal dominant pattern within a single family have been reported; CH may be autosomal dominant in about 5% of cases. [3]
Several factors have been shown to provoke CH attacks. Subcutaneous injection of histamine provokes attacks in 69% of patients. Stress, allergens, seasonal changes, or nitroglycerin may trigger attacks in some patients. Alcohol induces attacks during a cluster but not during remission. About 80% of CH patients are heavy smokers, and 50% have a history of heavy ethanol use.
Risk factors for CH include the following:
-
Male sex
-
Age older than 30 years
-
Small amounts of vasodilators (eg, alcohol)
-
Previous head trauma or surgery (occasionally)
Epidemiology
The exact prevalence of cluster headache (CH) in the United States is unknown; Kudrow estimated it to be 0.4% in men and 0.08% in women. [7] Its occurrence varies across geographical regions and has been reported to be as high as 1 in 500. [8, 9, 10, 11] Compared with classic migraine, CH is relatively uncommon, with an incidence equivalent to only 2–9% of that of migraine. Prevalence in males is 0.4–1%. In an extensive study of 100,000 inhabitants of the republic of San Marino, the prevalence was 0.07%. The incidence of CH in the United Kingdom is equivalent to that of multiple sclerosis.
Age-, sex-, and race-related demographics
Age of onset is usually 20–40 years, [3] however, CH has been reported in patients as young as 1 year and as old as 79 years.
For unknown reasons, men are afflicted by CH three times more often than are women. [3] Presentations in females may differ from those in males, according to data from the United States Cluster Headache Survey. [12] For example, women tend to develop CH at an earlier age and are also more likely to exhibit a second peak of CH incidence after the age of 50.
Racial and ethnic differences have not been well studied, but CH may be slightly more prevalent in African Americans and may be underdiagnosed in black women.
Prognosis
Generally, cluster headache (CH) is a lifelong problem. Potential outcomes include the following:
-
Recurrent attacks
-
Prolonged remissions
-
Possibility of transformation of an episodic cluster to a chronic cluster and vice versa
About 80% of patients with episodic CH maintain the episodic form of the disorder. In 4-13%, episodic CH eventually transforms into chronic CH. Intermediate (mixed) forms may also develop. Prolonged, spontaneous remissions occur in as many as 12% of patients, particularly in those with episodic CH. Chronic CH is more relentless and may persist in this form in as many as 55% of cases. Less frequently, chronic CH may remit into an episodic form.
No reported mortality is directly associated with CH. However, patients with CH are at increased risk for self-injury during attacks, suicide attempts, alcohol use (and other forms of substance abuse), cigarette smoking, and peptic ulcer disease. Suicides have been reported in cases where attacks are frequent and severe. The intensity of the attacks often leads CH patients to miss time from activities such as work or school. Medications used may have side effects, including the unmasking of coronary artery disease.
Pharmacologic intervention may play a part in the transformation of chronic CH into the episodic form; otherwise, it does not influence outcome. Late onset of the disorder, male sex, and previous episodic CH all predict a less favorable course.
Patient Education
Patients should be educated regarding the need to avoid known precipitants of cluster headache (CH). In addition, they should be instructed to avoid high altitudes.
For patient education resources, visit WebMD and the American Migraine Foundation.
-
Cluster headache: Functional imaging shows activation of specific brain areas during pain. Courtesy of Wikipedia Commons.
-
Cluster headache (CH): Voxel-based morphometry (VBM) structural imaging shows specific brain area of CH patients' (hypothalamus) being different to non-CH patients' brains. Courtesy of Wikipedia Commons.
-
Non-rebreather oxygen mask with reservoir for the acute treatment of cluster headache. Courtesy of Wikipedia Commons.







