Background
In 1724, Dr Hermann Boerhaave described the first, and likely most well known, case of esophageal perforation. Baron Jan von Wassenaer, the Grand Admiral of Holland, followed a large meal with his customary bout of emetic-induced vomiting. However, on this occasion, the Admiral experienced a sudden and severe pain in his upper abdomen after violent but minimally productive retching. Dead less than 24 hours later, his autopsy revealed a transverse tear of his distal esophagus and gastric contents in the pleural spaces. [1] Spontaneous esophageal rupture is a rare and dangerous entity, which today is commonly known as Boerhaave syndrome.
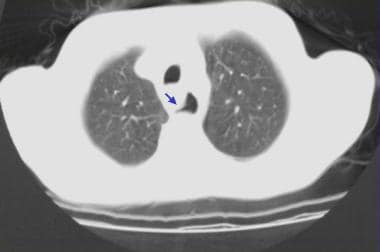
Today, most instances of esophageal perforation are iatrogenic, but this remains a potentially devastating condition. Rapid diagnosis and therapy provide the best chance for survival; however, delay in diagnosis is common, resulting in substantial morbidity and mortality. [2] This article discusses the causes, investigation, and initial therapy for this potentially lethal gastrointestinal condition. See the image below.
Pathophysiology
The esophagus is more vulnerable than the rest of the alimentary tract due to the lack of a serosal layer, which provides stability through elastin and collagen fibers. Perforation may be due to several mechanisms, including direct piercing, shearing along the longitudinal axis, bursting from radial forces, and thinning from necrosis of the esophageal wall.
Iatrogenic injury through esophageal instrumentation is the leading cause of perforation by either piercing or shearing and may be due to any number of procedures, especially endoscopy and dilatation of strictures. Such tears often occur near the pharyngoesophageal junction where the wall is weakest. Because the esophagus is surrounded by loose stromal connective tissue, the infectious and inflammatory response can disseminate easily to nearby vital organs, thereby making the esophageal perforation a medical emergency and increasing the likelihood of serious sequelae. Older age (>65 y) and underlying esophageal disease (tumor, stricture) predisposes toward perforation with instrumentation, which often occurs distal to the affected area. Perforation during surgery most often occurs in the abdominal esophagus.
Spontaneous esophageal rupture (Boerhaave syndrome) occurs secondary to a sudden increase in intraluminal pressures, usually due to violent vomiting or retching, and often follows heavy food and alcohol intake. In more than 90% of cases, perforation occurs in the lower third of the esophagus; most frequently, the tear is in the left posterolateral region (90%) and may extend superiorly. The predilection for left-side perforation is due to the lack of adjacent supporting structures, thinning of the musculature in the lower esophagus, and anterior angulation of the esophagus at the left diaphragmatic crus. Fifty percent of ruptures occur in patients with gastroesophageal reflux disease, suggesting that ease of pressure transfer from the abdominal to thoracic esophagus may facilitate rupture.
Shearing forces due to rapid increases in intragastric pressure against a closed pylorus result in a Mallory-Weiss tear (MWT). [3] These longitudinal mucosal lacerations occur most commonly at the gastroesophageal junction or gastric cardia, especially if a hiatal hernia is present, and often present with hematemesis. Ultimately, these tears can perforate if the pressure increases are unrelieved. Further discussion of MWTs is reserved for another section.
The cervical esophagus is the most common site of perforation by several other mechanisms as well, particularly in the region of the pyriform sinus. Trauma, almost uniformly penetrating, shows an affinity for the upper esophagus, while toxic ingestions and foreign bodies can directly damage the cervical esophagus or become lodged and cause insidious erosion of the muscle wall.
Etiology
Iatrogenic causes
Iatrogenic etiologies predominate the causes of esophageal perforation, accounting for more than 50% of cases. [3] Instrumentation modalities commonly include endoscopy, sclerotherapy, variceal ligation, pneumatic dilation, bougienage, and laser treatment. Placement of endotracheal, nasogastric, and Blakemore tubes represent less common iatrogenic causes.
Boerhaave syndrome
Boerhaave syndrome consistently accounts for about 15% of all perforations, normally secondary to vomiting after heavy food and alcohol intake, but possible by any action that abruptly increases intra-abdominal pressure against a closed superior esophageal sphincter. [4]
Foreign bodies
Swallowed foreign bodies may directly injure the esophagus by penetrating the tissue or becoming lodged at a point of esophageal narrowing, leading to pressure necrosis and wall weakness; pills and coins are common culprits. Ingestion of caustic chemicals may lead to direct wall inflammation and damage.
Trauma
Trauma represents an important cause of perforation, estimated at up to 10% of cases. Penetrating trauma is much far more prevalent than blunt, often in the form of knife or gun wounds, and is associated with significant injury to important adjacent cervical structures. [5] Blunt trauma may affect any portion of the esophagus, and the diagnosis is often delayed secondary to other injuries. [6]
Intraoperative esophageal perforation
Intraoperative esophageal perforation is a recognized complication of surgery, especially cardiothoracic or fundoplication, accounting for around 2% of all perforations. [7]
Epidemiology
United States data
Boerhaave syndrome is rare, accounting for 15% of all cases of esophageal perforation.
Iatrogenic causes account for 50-75% of esophageal perforations. The actual incidence depends on the procedure; rigid endoscopy carries a perforation rate 0.1-0.4%, while that of flexible endoscopy varies from 0.01-0.06%. Rates increase quickly when interventions are undertaken, such as pneumatic balloon dilatation in achalasia (2-6%) [8] or any procedure involving strictures secondary to radiation or tumor (15%). [9] Furthermore, the rate of perforation is increased in the presence of a large hiatal hernia or esophageal diverticula.
Penetrating trauma to the neck (2-9%), thinning of esophageal membrane secondary to variceal sclerotherapy (1-3%), and foreign body or toxic ingestions (5-15%) make up the bulk of the remaining causes.
Race-, sex-, and age-related data
No information on racial predilection is available.
Boerhaave syndrome is generally associated with vomiting and customarily occurs after drinking and eating binges. It is more commonly observed in males than in females. Iatrogenic perforation shows no predilection.
Boerhaave syndrome is most common among patients aged 40-60 years old, but isolated case reports in children have been described. [10]
Iatrogenic perforations are associated with preexisting pathology and so are more common in fifth and later decades of life.
Prognosis
The prognosis can be poor, especially if diagnosis is delayed. Even with prompt diagnosis and definitive therapy, the hospital course may be prolonged with high rates of morbidity and mortality.
The prognosis of cervical iatrogenic perforation is far better than that of spontaneous perforation.
Morbidity/mortality
Even with prompt therapy and advances in surgical technique, the mortality rate can be very high, varying from 5-75%; higher rates correlate with delays in both presentation and diagnosis.
Mortality also varies by etiology and location of the perforation. The highest rates are attributed to Boerhaave syndrome (up to 72%), partly because of the difficulty in making the diagnosis, followed by iatrogenic (19%) and traumatic perforations (7%). Cervical perforations portend a lower mortality compared with abdominal and thoracic perforations due to containment of potential contamination by tight fascial attachments and mechanisms, which may make injury more obvious.
Treatment delays and misdiagnosis of the condition contribute significantly to higher rates of morbidity and mortality. [2, 11] Diagnostic errors are prevalent, and esophageal ruptures can be confused with equally serious conditions such as acute myocardial infarction, perforated peptic ulcers, and acute pancreatitis.
The morbidity and mortality in esophageal perforation is most often due to an overwhelming inflammatory response to gastric contents in the mediastinum, pleural spaces, and adjoining tissues, as well as swift spread of infection to paraesophageal structures. Negative intrathoracic pressure may draw gastric material out of the esophagus, exacerbating injury.
Morbidity may be due to pneumonia, mediastinitis, empyema, polymicrobial sepsis, and multiorgan failure.
Complications
Complications include pneumonia, mediastinitis, sepsis, empyema, and adult respiratory distress syndrome.
Because of improved management, a significant number of patients now survive; recurrent spontaneous ruptures of the esophagus have been described. [12]
Esophageal injuries secondary to penetrating trauma often involve adjacent structures such as the spinal cord and trachea.
-
Esophageal Rupture and Tears in Emergency Medicine. Nonenhanced CT scan through the mid esophagus in a patient with esophageal perforation after upper GI endoscopy shows a false tract emanating from the esophagus (arrow).
-
Esophageal Rupture and Tears in Emergency Medicine. Nonenhanced CT scan through the mid esophagus in a patient with esophageal perforation after upper GI endoscopy shows leakage of oral contrast material (blue arrow) and air in the posterior mediastinum (red arrow).
-
Esophageal Rupture and Tears in Emergency Medicine. Water-soluble contrast esophagram from a patient with esophageal perforation after esophageal dilation shows contrast leak (arrowheads) and normal esophageal lumen (arrows).