Background
Epidermoid cysts represent the most common cutaneous cysts. While they may occur anywhere on the body, they occur most frequently on the face, scalp, neck, and trunk. [1, 2, 3]
Historically, epidermoid cysts have been referred to by various terms, including follicular infundibular cysts, epidermal cysts, and epidermal inclusion cysts. The term epidermal inclusion cyst refers specifically to an epidermoid cyst that is the result of the implantation of epidermal elements in the dermis. Because most lesions originate from the follicular infundibulum, the more general term epidermoid cyst is favored. The term sebaceous cyst should be avoided because it implies that the cyst is of sebaceous origin. Finally, the term milia refers to very small, superficial epidermoid cysts.
Epidermoid cysts are benign lesions; however, very rare cases of various associated malignancies have been reported. [4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15]
Pathophysiology
Epidermoid cysts result from the proliferation of epidermal cells within a circumscribed space of the dermis. Analysis of their lipid pattern demonstrates similarities to the epidermis. In addition, epidermoid cysts express cytokeratins 1 and 10, which are constituents of the suprabasilar layers of the epidermis. The source of this epidermis is nearly always the infundibulum of the hair follicle, as evidenced by the observation that the lining of the 2 structures is identical. [15]
Inflammation is mediated in part by the horny material contained in epidermoid cysts. Extracts of this material have been shown to be chemotactic for polymorphonucleocytes.
Studies have suggested that human papillomavirus (HPV) and exposure to ultraviolet light (UV) may play a role in the formation of some epidermoid cysts, particularly verrucous cysts with coarse hypergranulosis. [16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27]
The manner in which carcinomas may arise within epidermoid cysts is unclear. In a series of epidermoid cysts with carcinoma, immunohistochemical results for HPV were negative, suggesting that HPV is not likely to play a role in the development in squamous cell carcinoma (SCC) in epidermoid cysts. Chronic irritation or repetitive trauma to the epithelial lining of the cyst has been suggested to play a role in malignant transformation; however, this relationship has not been established. [28]
Etiology
Epidermoid cysts likely form by several mechanisms. They may result from the sequestration of epidermal rests during embryonic life, occlusion of the pilosebaceous unit, or traumatic or surgical implantation of epithelial elements. HPV infection, ultraviolet exposure, and eccrine duct occlusion may be additional factors in the development of palmoplantar epidermoid cysts. [29] HPV has also been identified in nonpalmoplantar epidermoid cysts.
Congenital epidermoid cysts of the anterior fontanelle or those that are orogenital in location presumably result from sequestration or trapping of epidermal rests along embryonic fusion planes during development. Lip and lingual lesions may be related to aberrant fusion of the branchial arches, while genital lesions may result from improper closure of the genital folds.
Any benign or malignant process affecting or growing near the pilosebaceous unit may lead to occlusion or impingement of the follicular ostia with subsequent formation of a cyst. Cysts with an acneiform distribution are likely the result of follicular occlusion. In elderly persons, accumulated sun damage can injure the pilosebaceous unit, causing abnormalities such as comedonal plugging and hypercornification, both of which can eventuate in cyst formation. [30] This condition is referred to as Favre-Racouchot syndrome.
True epidermal inclusion cysts result from the implantation of epithelial elements in the dermis. Certain injuries, especially of the crushing type, have been associated with subungual or terminal phalanx epidermoid cysts. A crush injury sustained from slamming a car door on a digit is frequently reported. Any surgical procedure can theoretically result in epidermoid cysts. Reports describe the formation of multiple epidermoid cysts after rhinoplasty, breast augmentation, and liposuction. [31] The use of dermal grafts, myocutaneous grafts, and needle biopsies has also been associated with the formation of epidermoid cysts.
Certain hereditary syndromes are associated with epidermoid cysts. Such syndromes include Gardner syndrome, [32] basal cell nevus syndrome, [5, 12, 27] and pachyonychia congenita. [33, 34] In addition, idiopathic scrotal calcinosis may actually represent an end stage of dystrophic calcification of epidermoid cysts. Note the image below.
Epidemiology
Race
No racial predilection has been identified. Pigmentation of epidermoid cysts is common in individuals with dark skin. In a study of Indian patients with epidermoid cysts, 63% of the cysts contained melanin pigment. [35]
Sex
Epidermoid cysts are approximately twice as common in men as in women.
Age
Epidermoid cysts may occur at any age; however, they most commonly arise in the third and fourth decades of life. Small epidermoid cysts known as milia are common in the neonatal period.
Prognosis
Epidermoid cysts are usually asymptomatic; however, they may become inflamed or secondarily infected, resulting in swelling and tenderness. Rarely, malignancies, including basal cell carcinoma, Bowen disease, SCC (most common of these rarities), mycosis fungoides, and melanoma in situ, have developed in epidermoid cysts. [15]
-
Unusually large epidermoid cyst with a prominent punctum on the back of a patient. (Ruler is in centimeters.)
-
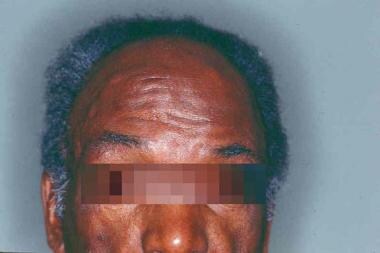
Multiple epidermoid cysts on the forehead of a patient with Gardner syndrome.
-
Cyst containing keratinous material (hematoxylin and eosin, original magnification X1.6).
-
Higher-magnification view of the cyst wall of the cyst in Media File 3 demonstrates a true epidermis with a granular layer and adjacent laminated keratinous material (hematoxylin and eosin, original magnification X20).