Overview
Dermatologic manifestations are seen in 25% of patients with sarcoidosis. They usually accompany systemic involvement, but in some cases they may be the only manifestations of the disease. Sarcoidosis is characterized by noncaseating epithelioid granulomas that may affect any organ system.
Although Jonathan Hutchinson described the first case in 1869, the etiology of the disease is still unknown. The disease most commonly involves granuloma formation in the lungs, with 90-95% of patients having some pulmonary involvement. Other commonly involved organ systems include the lymph nodes (especially the intrathoracic nodes), the skin, the eyes, the liver, the heart, and the nervous, musculoskeletal, renal, and endocrine systems. [1]
Physical Examination
Cutaneous involvement is classified as either "specific" or "nonspecific". Histopathologically, specific lesions manifest as noncaseating granulomas, whereas nonspecific lesions do not reveal granulomas on histopathologic examination. Erythema nodosum (EN) (shown below) is the main nonspecific cutaneous disease. Lupus pernio, maculopapular, nodular, scar, plaque, angiolupoid, ichthyosiform, lichenoid, annular, verrucous, psoriasiform, and ulcerative lesions and subcutaneous nodules are examples of specific cutaneous disease.
Blau syndrome and early-onset sarcoidosis represent familial and sporadic forms of pediatric granulomatous autoinflammatory disease caused by mutations in the NOD2 gene. Clinical onset is usually early in life, with noncaseating granulomas affecting the skin, joints, and uveal tract. [2, 3]
Erythema nodosum
EN is a hypersensitivity reaction resulting from exposure to a variety of infectious agents (especially recent streptococcal infection), drugs (including oral contraceptives), or systemic inflammatory disorders (eg, sarcoidosis, inflammatory bowel disease). EN is usually an acute, self-limiting process and rarely requires treatment. Recurrences are uncommon. Tender, erythematous nodules are usually present on the extremities, most commonly on the anterior surface of the tibia. Fever, arthralgia, and malaise may occur. EN is more common in European, especially Scandinavian, women of childbearing age than in other people.
Loefgren syndrome
Löfgren syndrome is classically described as a triad of EN, polyarthritis, and hilar adenopathy. The adenopathy may be unilateral or bilateral hilar and/or right paratracheal lymphadenopathy. Other symptoms include anterior uveitis, fever, ankle periarthritis, arthralgias, and pulmonary involvement.
Löfgren syndrome is usually an acute disease with an excellent prognosis, typically resolving spontaneously from 6-8 weeks to up to 2 years after onset. Pulmonologists, ophthalmologists, and rheumatologists often define this syndrome differently, describing varying combinations of arthritis, arthralgia, uveitis, EN, hilar adenopathy, and/or other clinical findings. (See the image below.)
Lupus pernio
Lupus pernio, first described by Besnier in 1889, is a striking manifestation of sarcoidal skin lesions. Lupus pernio is characterized by red to purple or violaceous, indurated plaques and nodules that usually affect the nose, cheeks, ears, and lips, but it can appear on the dorsa of the hands, and on the fingers, toes, and forehead. (See the images below.)
Lupus pernio is usually more common in black women with long-standing systemic, usually pulmonary, sarcoidosis than in other people. It is also commonly seen with chronic uveitis and bone cysts. The course is usually chronic, may be more recalcitrant to treatment, and may result in severe cosmetic disfigurement. Lupus pernio, especially involving the nasal rim, has been associated with granulomatous involvement of the upper respiratory tract (50%) and lungs (75%). Additionally, it is associated with a higher frequency of ocular involvement, bone cyst formation, and lymphadenopathy or organomegaly. [4]
Macular sarcoidosis
Macular or papular sarcoidosis is the most common lesion seen in cutaneous sarcoidosis, especially in black women. Granulomatous acne rosacea may mimic sarcoidosis clinically and histopathologically. Usually, lesions are asymptomatic, red-brown macules and papules commonly involving the face, the periorbital areas, the nasolabial folds, and/or the extensor surfaces. Lesions usually resolve without scarring, although scarring may occur. These lesions may also occur in acute sarcoidosis. (See the image below.)
The use of dermoscopy to aid in the clinical diagnosis of macular and plaque-type sarcoidosis has been reported, with findings of "translucent yellow to orange globular-like or structureless areas associated with linear vessels" and being associated with granulomatous skin disease, including cutaneous sarcoid. [5] Widespread atrophic lesions with elastolysis have been reported, and widespread lichenoid lesions may resemble erythroderma. [6, 7]
Plaque sarcoidosis
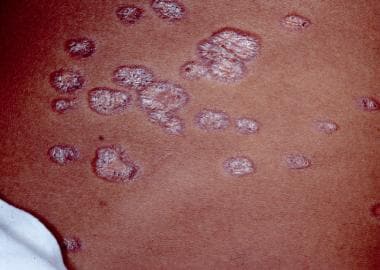
Plaque sarcoidosis is characterized by round to oval, red-brown to purple, infiltrated plaques; the center of the plaque may be atrophic (see the image below). Some plaques may even appear scaly and can be confused with lesions of psoriasis or lichen planus. Dermoscopy may aid in the clinical diagnosis, as noted above.
The lesions most commonly occur on the extremities, face, scalp, back, and buttocks, and they may have an annular appearance (see the image below). The distribution is usually symmetrical. Angiolupoid sarcoidosis is a subtype that has a similar appearance but has large, telangiectatic vessels in addition to the characteristics mentioned above. This form of cutaneous involvement is usually chronic; most patients have the disease for more than 2 years. Lesions can heal with scarring, and, if plaques involve the scalp, they may lead to alopecia. Patients with plaque lesions usually have more severe systemic involvement.
Subcutaneous nodular sarcoidosis
Subcutaneous nodular sarcoidosis is also called Darier-Roussy sarcoidosis. Lesions are usually nontender, firm, oval, flesh-colored or violaceous nodules that are 0.5-2 cm in diameter. They are commonly found on the extremities or trunk. These lesions usually appear in the beginning of the disease. Patients with these lesions often have nonsevere systemic disease. In some patients, the nodules resolve spontaneously. [8, 9]
Other lesions
Sarcoidosis is called the "great imitator" because it can have almost any morphology. [10] Other rare lesions of cutaneous sarcoidosis are ichthyosiform, [11] lichenoid, vasculitic, [12] psoriasiform, erythrodermic, verrucous, papillomatous, and ulcerative lesions. (See the image below.)
Scar and tattoo infiltration
Infiltration of scars may occur (see the image below). Scars from previous trauma, surgery, venipuncture, or tattoo may become infiltrated and show a red or purple color. These lesions may be tender.
The development of sarcoidal lesions within tattoos has been well documented, although hypersensitivity granulomatous reactions to tattoo pigment need to considered in the differential diagnosis and should be considered in the context of the overall clinical presentation of the sarcoid patient. Specific tattoo pigment colors may be targeted more than others, even within the same patient with a multicolored tattoo. [13]
Differential Diagnosis
Dermatologic conditions to consider in the differential diagnosis of sarcoidosis include the following:
-
Cutaneous tuberculosis
-
Drug eruptions
-
Granuloma annulare
-
Granuloma faciale
-
Lamellar ichthyosis
-
Leprosy
-
Lichen planus
-
Discoid lupus erythematosus
-
Subacute cutaneous lupus erythematosus
-
Lymphocytoma cutis
-
Necrobiosis lipoidica
-
Plaque psoriasis
-
Syphilis
-
Tinea corporis
B-cell lymphoma, foreign body reaction (including hypersensitivity granulomatous reaction to tattoo pigment), and lichen planopilaris should also be considered in the differential diagnosis. Silica granulomas are often associated with sarcoidosis, and patients on targeted immunotherapy for melanoma may develop sarcoidal granulomas. [14, 15, 16, 17]
Kveim-Siltzbach Test and Tuberculin Skin Test
Kveim-Siltzbach test
The Kveim test is the most specific test for sarcoidosis. It is not commonly available, nor commonly used, because of difficulty in obtaining a validated antigen source, as well as a fear of transmitting infection. The Kveim test involves intradermal injection of tissue from the spleen or the lymph node of a patient with sarcoidosis. A biopsy sample is obtained from the area 4-6 weeks after injection and is histologically examined for noncaseating granuloma formation, which, if found, indicates a positive result.
Tuberculin skin test
Regarding the tuberculin skin test, patients with sarcoidosis have impaired delayed-type immune reactions. Two thirds of patients with systemic sarcoidosis have cutaneous anergy to the tuberculin and other skin tests. It is not known if cutaneous anergy is frequent in patients with cutaneous lesions of sarcoidosis with little or no systemic involvement.
Biopsy
The skin is the most easily accessible tissue for biopsy and is extremely helpful in supporting the diagnosis of sarcoidosis. Biopsy of erythema nodosum, however, is less helpful as it is not specific for sarcoidosis. Biopsy specimens need to be sent for histologic examination, and staining may need to be performed to rule out infectious causes of granuloma formation, including mycobacterial and deep fungal infections. Tissue culture may be appropriate in some clinical settings, especially if fungal or atypical mycobacterial infections are suspected.
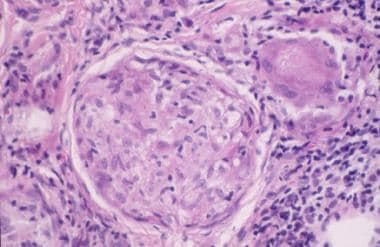
Histologic Findings
Typical sarcoid lesions are characterized as “naked,” noncaseating granulomas. Granulomas are referred to as naked because they only have a sparse lymphocytic infiltrate at the margins of granulomas. The granulomas are generally circumscribed and composed of epithelioid cells with little or no necrosis. Fibrosis, if present, usually starts at the periphery and advances toward the center. Granulomas are usually in the superficial dermis, but they may involve the thickness of the dermis and extend to the subcutaneous tissue. (See the image below.)
Islands of epithelioid cells may contain a few Langhans giant cells. Giant cells may contain asteroid or Schaumann bodies. Asteroid bodies are star-shaped eosinophilic structures. Schaumann bodies are round or oval, laminated structures that are usually calcified at the periphery.
Pharmacologic Therapy
The need for medical therapy varies based on the symptoms and the organ systems involved in each patient. Oral corticosteroids are usually the treatment of choice for patients with hypercalcemia and for those with serious end-organ involvement, such as symptomatic stage II and all stage III pulmonary disease, as well as for patients with neurologic, cardiac, or ocular involvement. As opposed to the more severe systemic involvement requiring oral therapy, Löfgren syndrome is usually an acute process that is self-limited and that resolves without immunosuppressive treatment in weeks. Symptomatic relief can be obtained using nonsteroidal anti-inflammatory drugs (NSAIDs) or relatively low doses of corticosteroids.
Limited, nondisfiguring cutaneous involvement may be treated with topical or intralesional corticosteroids. Intralesional injections of 2-10 mg/mL [18] of triamcinolone acetonide can be used at monthly intervals. More chronic skin lesions, such as plaques or lupus pernio, require more aggressive therapy because they can lead to permanent scarring.
If intralesional corticosteroids are not effective, other standard therapies include systemic corticosteroids, low-dose oral or subcutaneous methotrexate, [19, 20, 21] or antimalarials (hydroxychloroquine [22] and chloroquine). [23] Anti–tumor necrosis factor (TNF)–alpha therapy and other biological agents represent promising options for patients with recalcitrant or disfiguring disease. [18, 24, 25, 26, 27, 28] It should also be noted that anti-TNF agents have produced granulomatous eruptions. [29]
Other agents that have been used to treat cutaneous sarcoidosis include the following:
-
Cyclosporine
-
Chlorambucil [33]
-
Oral isotretinoin [34]
-
Allopurinol [35]
-
Doxycycline
-
Tetracycline
-
Psoralen with ultraviolet A (UVA)
-
Etanercept
-
Leflunomide
-
Pentoxifylline
-
Melatonin [41]
-
Janus kinase (JAK) inhibitors [44]
-
Topical Ganoderma lucidum (Reishi mushroom) [45]
-
Combination prednisone and hydroxychloroquine [46]
One case report describes remission of sarcoidosis after the patient was placed on an angiotensin-converting enzyme (ACE) inhibitor. [47] Another report describes improvement in two cases using photodynamic therapy with methyl aminolevulinate (Metvix). [48] Intralesional 5-fluoruracil has been used successfully. [49]
Radiation and Surgical Treatment
In terms of nonpharmacologic therapy, radiation has been used in cases of treatment-resistant cutaneous lesions. [50]
Surgical resection of smaller, severely disfiguring and recalcitrant lesions may be attempted. The risk of lesion recurrence and hypertrophic and keloidal scarring does exist. Laser surgery using carbon dioxide [51] and pulsed dye laser has also been used in the treatment of disfiguring skin plaques and lupus pernio. [18]
Additional Treatment Considerations
Inpatient care
Inpatient care is rarely needed for patients with cutaneous disease. However, in patients with respiratory insufficiency, hospitalization may be needed. Complications of systemic immunosuppressive therapy, namely severe infection, may result in hospitalization.
Consultations
Early involvement of other clinicians, such as an ophthalmologist, an internist, a rheumatologist, and a pulmonologist, for monitoring other organ systems that may be involved is recommended. Choice of consultation specialist is driven by symptoms and end-organ of involvement.
Long-term monitoring
Follow-up care should be frequent for the first 2 years after diagnosis. Patients with stage I disease can receive follow-up care twice yearly, whereas patients with more advanced lung disease should be seen more frequently. All patients should be monitored for at least 3 years after discontinuation of therapy.
During follow-up care, patients should have a history with a review of systems and should undergo physical examination, chest radiography, and pulmonary function tests to evaluate for active or insidiously progressive disease. A baseline electrocardiogram is of use to assess for cardiac involvement and for future comparison if symptoms develop. Baseline laboratory examination may include calcium and vitamin D levels as calcium dysregulation with hypercalcemia may occur. In general, an angiotensin-converting enzyme (ACE) level has limited usefulness as a diagnostic test for sarcoidosis.
Ophthalmologic assessment is needed initially—generally annually in all patients and more frequently in those with ocular involvement. Therapeutic use of hydroxychloroquine (Plaquenil) may also warrant more frequent, detailed ophthalmologic examinations.
A large review by Ji et al of the Swedish Hospital Registry noted an elevated risk of skin cancer (especially squamous cell carcinoma), non-Hodgkin lymphoma, and leukemia in hospitalized patients with sarcoidosis, extending beyond the first year after hospitalization. Therefore, close follow up for malignancies is recommended. [52]
Questions & Answers
Overview
What is the prevalence of dermatologic manifestations of sarcoidosis and how are they characterized?
How is cutaneous involvement in sarcoidosis classified?
What is the manifestation of Löfgren syndrome in sarcoidosis?
How is plaque sarcoidosis characterized?
What is the manifestation of erythema nodosum (EN) in sarcoidosis?
What is the manifestation of lupus pernio in sarcoidosis?
What is the manifestation of macular sarcoidosis?
How is subcutaneous nodular sarcoidosis characterized?
Why is sarcoidosis called the great imitator?
What is the association of sarcoid lesions with tattoos?
Which dermatologic conditions should be included in the differential diagnoses of sarcoidosis?
What is the role of the Kveim-siltzbach test in the diagnosis of sarcoidosis?
What is the role of the tuberculin skin test in the diagnosis of sarcoidosis?
What is the role of biopsy in the workup of sarcoidosis?
Which histologic findings are characteristic of sarcoidosis?
What is the role of pharmacologic therapy in the treatment of sarcoidosis?
What is the role of nonpharmacologic therapy in the treatment of sarcoidosis?
When is inpatient care indicated for the treatment of sarcoidosis?
Which specialist consultations are needed for the treatment of sarcoidosis?
What is included in long-term monitoring of patients with sarcoidosis?
-
Erythema nodosum.
-
Bilateral hilar lymphadenopathy.
-
Stage III pulmonary disease with pulmonary infiltrates.
-
Periocular papules and plaques.
-
Plaque sarcoidosis.
-
Erythematous papules on the knee.
-
Lupus pernio with nodules on the nasal tip and sidewall.
-
Annular sarcoidosis.
-
Sarcoidosis with infiltration of a scar.
-
Histopathologic features of sarcoidosis showing the hallmark noncaseating granulomas.
-
Cutaneous sarcoidosis. Violaceous papules or nodules of lupus pernio.